Übersetzt aus dem Englischen:
Erlernen Sie die Rekonstruktion des lateralen Sprunggelenksbandes nach der Chrismann-Snook-Technik mit Schritt-für-Schritt-Anleitungen auf OrthOracle. Unsere E-Learning-Plattform enthält hochauflösende Bilder und eine zertifizierte Fortbildung (CME) zur chirurgischen Vorgehensweise bei der Rekonstruktion des lateralen Sprunggelenksbandes nach der Chrismann-Snook-Technik.
Sprunggelenksinstabilität ist ein sehr häufiges Problem, bei dem es wichtig ist, zwischen funktioneller Instabilität und mechanischer Instabilität zu unterscheiden. Die überwiegende Mehrheit der Fälle tritt posttraumatisch auf, jedoch ist die Behandlung dieser Untertypen sehr unterschiedlich.
Funktionelle Instabilität bedeutet, dass die Ursache für die Symptome entweder eine schlechte neuromuskuläre Funktion, eine schlechte propriozeptive Funktion oder eine Pathologie innerhalb des Sprunggelenks ist, die ein plötzliches und schmerzhaftes „Nachgeben“ verursachen kann. Mechanische Instabilität ist seltener und bedeutet, dass die stabilisierenden Bandstrukturen um das Sprunggelenk herum defizitär sind und eine übermäßige und messbare Zunahme des Bewegungsumfangs im Sprunggelenk ermöglichen. Aus symptomatischer Sicht gibt es wenig, was zwischen diesen beiden Situationen unterscheidet. Bei Fällen mit mechanischer Instabilität kann jedoch eine Bandrekonstruktion erforderlich sein.
Nach einem akuten Umknicken mit Belastung und Supination heilt die überwiegende Mehrheit der Bänderverletzungen spontan mit konservativer Behandlung. Frühzeitig durchgeführte MRT-Untersuchungen sind nicht hilfreich, um vorherzusagen, ob eine Bandrekonstruktion erforderlich sein wird.
Original Intro:
Lateral ankle ligament reconstruction: Chrismann-Snook type technique
Learn the Lateral ankle ligament reconstruction: Chrismann-Snook type technique surgical technique with step by step instructions on OrthOracle. Our e-learning platform contains high resolution images and a certified CME of the Lateral ankle ligament reconstruction: Chrismann-Snook type technique surgical procedure.
Ankle instability is a very common problem and the key thing to appreciate is the difference between a functional instability and mechanical instability. The vast majority of cases occur post-traumatically, but the management of these sub-types is very different.
Functional instability means that the cause for symptoms is either poor neuromuscular function, poor proprioceptive function or pathology within the ankle joint which can cause an instantaneous and painful ‘giving way’. Mechanical instability is less common and means that the stabilising ligamentous structures around the ankle are deficient and are allowing excessive and measurable increase in the range of movement occurring at the ankle joint. From the symptomatic perspective, there is little that enables one to differentiate between these two different situations. The cases with mechanical instability though are those where ligament reconstruction may be required.
Following an acute weight bearing and inversion ankle sprain, the natural history in the vast majority of ligament injuries will spontaneously resolve with conservative management. MRI scans taken early on are not useful for prognosticating on whether ligament reconstruction will be required.
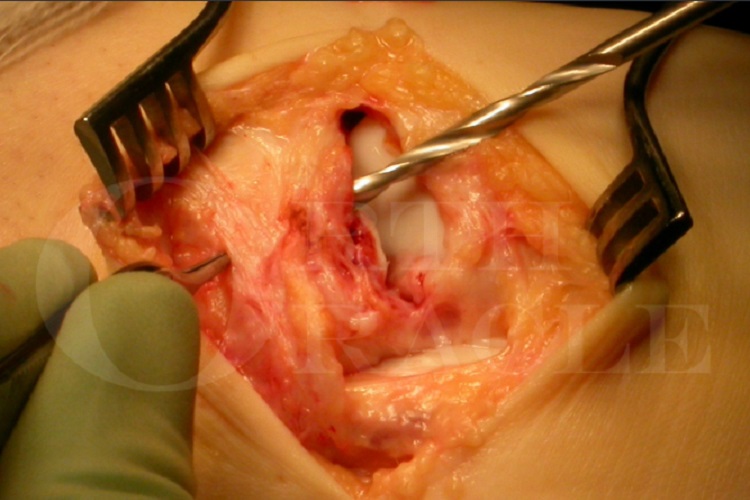
For those cases with true mechanical instability (which is often determined at the time of examination under anaesthetic), the most commonly performed primary lateral ligament reconstruction is the Brostrom, which tightens the lateral peri-fibular capsular tissue. Highly successful though this ligament reconstruction is, there are cases which require a more robust type of repair. These sorts of cases are patients with poor collagen subtype and generalised ligamentous laxity (one should always enquire about the start points of instability and if there is no defined trauma, then this should raise concerns). These patients will often also have other joint instabilities, commonly the patellofemoral joint and shoulders, wrists and joints of the hand. Using the native lateral ligament alone is likely to lead to early failure, even if the on-table reconstruction appears sound. Revision cases with poor remaining soft tissue, individuals of high BMI and potentially those involved in heavy manual type activities are also the type of cases where an alternative to the Brostrom may be required. Surgeons who are performing ankle replacement also require a means to robustly stabilise the lateral ankle if replacing the joint in cases of known instability or where a lateral instability occurs unexpectedly on-table following testing of the implanted joint.
Most commonly performed type of ankle ligament reconstruction in these circumstances is using a bone tunnel through the fibula.
The best known are the Evans reconstruction and Watson Jones, both of which provide stabilisation to ankle and subtalar joint by “non-anatomic” routing of the stabilising soft tissue structures through the fibula, and the Chrisman-Snook which seeks more closely to reconstruct the mechanical effects of the ATFL and CFL ligaments (see indications section for detail). There are various tissues that can be used including all or part of peroneus brevis, free hamstring autograft, free plantaris autograft or various manufactured neo ligaments as well as allograft material such as the Wright Graft Jacket demonstrated in this technique.
Author: Mark Herron FRCS
Institution: OrthOracle, London, UK.
zum AOUC-Angebot für OrthOracle