Learn the Brachial plexus injury: Supraclavicular and infraclavicular approaches surgical technique with step by step instructions on OrthOracle. Our e-learning platform contains high resolution images and a certified CME of the Brachial plexus injury: Supraclavicular and infraclavicular approaches surgical procedure.
The brachial plexus is an intricate and complex structure that connects the spinal nerves C5-T1 to their terminal nerve branches in the upper extremity through a complex series of interconnections and divisions.
Although there is extensive literature describing the brachial plexus in terms of its anatomy and physiology as well as its relationship to surrounding structures, for the surgeon dealing with injuries around the brachial plexus or other lesions that require visualisation of the brachial plexus, a safe and reliable technique for surgical approach is hugely valuable.
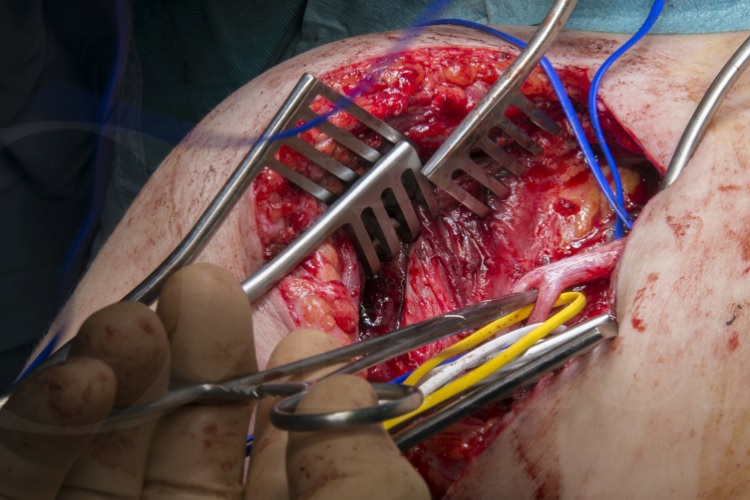
In this instructional technique I have highlighted the two major approaches to the brachial plexus; a supraclavicular approach, followed by an infraclavicular approach, keeping to the standard approaches with variations explained where relevant. Both approaches are required for the brachial plexus surgeon on a frequent basis. The description here is confined to the approach in an adult.
Clearly for a brachial plexus injury, the most important decision to be made is whether the brachial plexus requires exploration at all or whether the injury is one that would be expected to recover under observation, or perhaps is so severe that exploration will not offer any significant advantage over and above distal nerve transfers to reconstruct lost function where possible. This is clearly an extensive area of debate and discussion which is outside of the scope of this technical description.
If a pan-root avulsion can be confirmed without exploration, for example, on high resolution MRI imaging, many surgeons would now avoid a plexus exploration in such a scenario and look for reconstructive options involving extra plexoral donors and free muscle transfers, or explore prosthetic options, with or without limb amputation. Again, this is an area of debate and outside the scope of this technique.
The infra-clavicular plexus is less commonly explored in trauma where the injuries more often tend to be continuity lesions that recover. However, penetrating injuries in this area may require exploration and the brachial infraclavicular plexus may require protection or mobilisation as part of other surgical procedures around the shoulder. One particular scenario where this may be required is during a shoulder replacement or fixation after a fracture dislocation that has left the plexus injured. I have found a limited infraclavicular exposure of the plexus invaluable in performing highly selective neurectomies where in particular the pectoralis muscles may be involved in spasticity.
In my practice I have found a limited infraclavicular exposure of the plexus invaluable in performing highly selective neurectomies for spasticity following stroke or brain injury. In particular in these case, the pectoralis muscles may be involved in spasticity and their innervation can be directly accessed as it comes off the infraclavicular plexus into these muscles.
It is worth noting that there is considerable variation in the anatomy of the brachial plexus between individuals and a thorough knowledge of these potential variations is important in order to make a reliable diagnosis when confronted with injured components of the plexus. The most typical closed injury is a shoulder dislocation which can be a high energy injury causing huge disruption to surrounding neurovascular structures, or as is common in elderly patients, a low velocity injury with a dislocation, often combined with a fracture, where the injury to the cords can be widespread but of lower energy.
The supra-clavicular approach to the brachial plexus tends to be used in supraclavicular injuries that may involve ruptures to one of the trunks or roots of the plexus that may be reconstructable but also to define the extent of injury, which in many cases can only be established by a clear exploration and surgical diagnosis.
OrthOracle readers will find the following instructional techniques also of interest:
Brachial plexus injury: Thoracodorsal to triceps nerve transfer
Brachial plexus injury: reconstruction with intercostal to radial nerve transfer
Brachial plexus injury: Thoracodorsal nerve to long thoracic nerve transfer for scapula winging
Brachial plexus injury: exploration and long thoracic nerve decompression
Brachial plexus injury: Medial branch spinal accessory (XI) nerve transfer to Suprascapular nerve.
Author: Tahseen Chaudhry, Consultant Peripheral Nerve Surgeon
Institution: Queen Elizabeth Hospital Birmingham, UK.
Clinicians should seek clarification on whether any implant demonstrated is licensed for use in their own country.
In the USA contact: fda.gov
In the UK contact: gov.uk
In the EU contact: ema.europa.eu